By Sian Venables
Once thought to be a relatively mild mannered virus, Zika’s role in the development of severe foetal abnormalities has put it firmly on the public’s radar. With an epicentre in Brazil it has spread to over 40 countries, upsetting the Olympic games in Rio and causing a national outcry in the US when it required funding to be siphoned from the Affordable Care Act. Hurdles to its eradication arise because of its subtle symptoms and ease of transmission. Whether through targeting mosquitos or developing vaccines, there will be no single solution to quashing the Zika epidemic.
The WHO recently classed the outbreak as a “public-health emergency of international concern.”. Identified in Uganda in 1947, there had been only 14 documented cases of the virus until 2007, when the first epidemic swept through the Pacific Islands. It cropped up again in 2013 in French Polynesia before the latest outbreak in Brazil was postulated to have links to an infected traveller to the World Cup in Rio, 2014.
Public-health emergency of international concern
The virus itself manifests predominantly in Aedes mosquitos. Though bites from the infected insects are believed to be the commonest route of transmission, spread can also occur through sex, blood transfusions and, to devastating effect, from mother to child. Because the virus can be so harmless, asymptomatic carriers are hard to identify, making upsetting transmission a daunting task. In the French Polynesian out-break, blood banks were thrown into a frenzy; with testing for Zika not previously standard the CDC reported that ‘2.8% of blood donors tested positive’.
Zika’s spectrum of effects is seen in its most extreme form in pregnant women. Infections acquired in the first trimester are associated with the worst outcomes for developing children, so the challenge lies in rapidly identifying these cases. Generally presenting with only a rash, fever, joint pain and conjunctivitis, expectant mothers and hurried health care workers often attribute symptoms of the viral infection to pregnancy hormones.
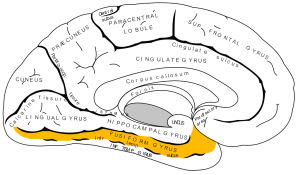
‘Mounting evidence from many studies’ links maternal Zika infection to the development of severe foetal microcephaly, states the CDC. The virus was identified both in the brains of miscarried micro-cephalic children and in the amniotic fluid of infected mothers (Calvet et al. 2016) It is thought to cause the disorder by proliferating in, and therefore damaging, cortical neural progenitor cells (which go on to form cortex) so is especially damaging to vulnerable, developing brains (Tang et al. 2016).
Though the effects of Zika have mainly been publicised as harmful to developing foetuses, more evidence is building to highlight negative outcomes of infection in children and mature adults. Presence of the virus is now described as a causal factor in the development of the autoimmune disorder Guillain-Barré (Cao-Lormeau et al. 2016). The condition is usually temporary, characterised by the body attacking its own nerves it presents with peripheral muscle wasting and paralysis. Occasionally it affects muscles that control breathing, a consequence that can prove fatal.
Cases of acute inflammation of the brain and spinal cord are also being examined as having a possible link to Zika infection. The development of these conditions means that neurologists will be key players in the fight against the virus, though they are in short supply in some of the worst affected areas.
108% spike in online orders of pregnancy terminating pills
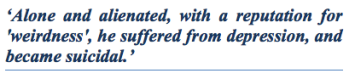
The virus’ spread has given rise to discussion of a taboo ethical dilemma in many of the worst hit countries where abortions are illegal. A case example is Brazil, where abortion is outlawed except in circumstances of rape, health emergencies or anencephaly. Activists are campaigning for laws to be loosened where Zika is a concerned, after an 108% spike in online orders of pregnancy terminating pills in affected areas (Aiken et al. 2016).
This surge in demand for abortions is suspected to be underestimated, as some women in helpless situations resort to unsafe, underground terminations. The task of caring for a severely disabled child is realised as emotionally and often economically unfeasible for many living in already deprived circumstances. The epidemic is not set to die down any time soon, so providing access to safe abortions is an issue that needs to be addressed with an open mind by governments and religious leaders alike, if we are to protect affected women from the social and often fatal consequences of illegal abortions.
With a tried and tested vaccine years from completion, swift reactions to tackling Zika are predominantly focussing on thwarting transmission. Compliance with public health advice about abstinence in pregnancy and avoiding unprotected sex, as well as covering up to avoid mosquito bites at dusk and dawn, are key to keeping infection rates low. A pioneering $18 million project is currently on the go, with intent to release “mutant mosquitos” infected with Wolbachia bacteria into the worst affected areas of Brazil. The bacteria has been reported to transform Aedes aegypti mosquitoes, making them ‘highly resistant’ to two forms of Zika virus, to the extent that they no longer harbour the virus in their saliva (Dutra et al. 2016).
The spread of Zika is likely to be exacerbated by a rise in global temperatures and the unstoppable force of globalisation. With ever more interconnected societies comes a shared responsibility to address the ethical dilemmas and financial burdens of treating infectious diseases. How we handle this outbreak will set a precedent for the inevitable onslaught of epidemics that will come from rising anti-biotic resistance. Zika’s devastating effects can and will be thwarted, but how much pressure is put on governments to treat it as a priority will determine how quickly the battle is won.
If the many dilemmas raised by Zika are of interest to you Medsin urges you to come to a talk hosted by the Hispanic society on the 10th of November: ‘Zika virus: From obscurity to threat’. The event will take place from 6-8pm in School 6 of St Salvator’s quad. We hope to see you there!
Bibliography
Aiken, A.R.A. et al., 2016. Requests for Abortion in Latin America Related to Concern about Zika Virus Exposure. New England Journal of Medicine, 375(4), pp.396–398.
Calvet, G. et al., 2016. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. The Lancet Infectious Diseases, 16(6), pp.653–660.
Cao-Lormeau, V.-M. et al., 2016. Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. The Lancet, 387(10027), pp.1531–1539.
Dutra, H.L.C. et al., 2016. Wolbachia Blocks Currently Circulating Zika Virus Isolates in Brazilian Aedes aegypti Mosquitoes. Cell host & microbe, 19(6), pp.771–4.
Tang, H. et al., 2016. Zika Virus Infects Human Cortical Neural Progenitors and Attenuates Their Growth Brief Report Zika Virus Infects Human Cortical Neural Progenitors and Attenuates Their Growth. Cell Stem Cell, pp.1–4.


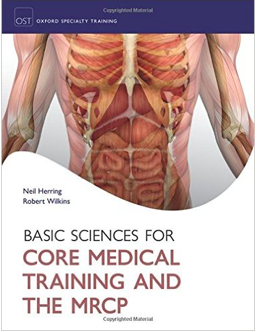 ford university press, comes a new textbook designed specifically, or so it seems, for the pre-clinical St Andrews student. Using the same systems-based approach, with integrated clinical relevance that our curriculum throws at us, this brand new book clearly lays out all the basic science necessary for the typical honors student. But how does the book really perform next to the average recommended medical booklist?
ford university press, comes a new textbook designed specifically, or so it seems, for the pre-clinical St Andrews student. Using the same systems-based approach, with integrated clinical relevance that our curriculum throws at us, this brand new book clearly lays out all the basic science necessary for the typical honors student. But how does the book really perform next to the average recommended medical booklist? Oxford Cases in Medicine and Surgery promises to be unique in that it’s goal is essentially to teach students how to think clinically without needing to be in a clinical setting. Different, but very common presenting complaints are the focus of each chapter, or ‘Core Case’ as they have been titled. Each Core Case begins by stating the name, age and presenting complaint of a patient and then, based solely on that information, asks you to think critically and identify all possible serious causes that you need to rule out first. Sound like something every medical student needs to know how to do when they get out on the wards? Definitely. However, instead of throwing you in the deep end filled with anxiety, as you would feel on a ward with an actual patient, Oxford Cases gives you mnemonics and walks you through all of the red flags you should be looking out for. This text teaches you how to evaluate patients’ presenting complaints in a systematic way that ensures you won’t be missing anything vital and are covering all possibilities efficiently.
Oxford Cases in Medicine and Surgery promises to be unique in that it’s goal is essentially to teach students how to think clinically without needing to be in a clinical setting. Different, but very common presenting complaints are the focus of each chapter, or ‘Core Case’ as they have been titled. Each Core Case begins by stating the name, age and presenting complaint of a patient and then, based solely on that information, asks you to think critically and identify all possible serious causes that you need to rule out first. Sound like something every medical student needs to know how to do when they get out on the wards? Definitely. However, instead of throwing you in the deep end filled with anxiety, as you would feel on a ward with an actual patient, Oxford Cases gives you mnemonics and walks you through all of the red flags you should be looking out for. This text teaches you how to evaluate patients’ presenting complaints in a systematic way that ensures you won’t be missing anything vital and are covering all possibilities efficiently.





 practice safely on patients. For many of us, it can be difficult to ascertain where to begin in this learning process.
practice safely on patients. For many of us, it can be difficult to ascertain where to begin in this learning process.  Each book integrates a system’s core biomedical science with its clinical
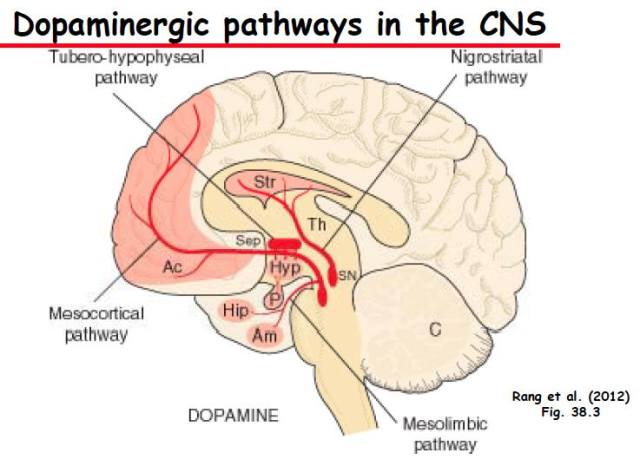
Each book integrates a system’s core biomedical science with its clinical The initial storytelling is succeeded by several chapters detailing the most common pathology, where the standard of clear, smooth-flowing, writing, is upheld. These entail the epidemiology, aetiology, pathogenesis, clinical features, diagnostic approach, and medical and surgical management, for a broad range of commonly encountered conditions – as well as a chapter dedicated to emergencies. A public health approach is integrated; for instance, the diagnosis of respiratory disease is intimately linked with a patient’s occupational history, and this is both appreciated and expounded upon in ‘Respiratory Medicine’. Pharmacological interventions are also covered, if not to a depth where their molecular mechanisms are elucidated. Clinical cases are routinely incorporated, and sometimes through realistic ‘graphic narratives’, which are enjoyable to trace. Each chapter is prefaced by a number of thought-provoking questions, that if paid attention to, prompt the reader to actively seek answers – such as ‘What investigations are useful for someone presenting with chronic dyspnoea?’ or ‘What factors determine the surgical approach in a woman shown to have breast cancer?’
The initial storytelling is succeeded by several chapters detailing the most common pathology, where the standard of clear, smooth-flowing, writing, is upheld. These entail the epidemiology, aetiology, pathogenesis, clinical features, diagnostic approach, and medical and surgical management, for a broad range of commonly encountered conditions – as well as a chapter dedicated to emergencies. A public health approach is integrated; for instance, the diagnosis of respiratory disease is intimately linked with a patient’s occupational history, and this is both appreciated and expounded upon in ‘Respiratory Medicine’. Pharmacological interventions are also covered, if not to a depth where their molecular mechanisms are elucidated. Clinical cases are routinely incorporated, and sometimes through realistic ‘graphic narratives’, which are enjoyable to trace. Each chapter is prefaced by a number of thought-provoking questions, that if paid attention to, prompt the reader to actively seek answers – such as ‘What investigations are useful for someone presenting with chronic dyspnoea?’ or ‘What factors determine the surgical approach in a woman shown to have breast cancer?’